What you need to know about children's eyes

Children's eyes are not very different from adult eyes. For me, as a doctor, the most important difference is that an adult usually guesses that if you pull a goat from your nose, pick it up with your hand in that dirty pipe, then eat a cheburek from Belorussky Station, stroke a homeless or a doggy, then scratch it probably not worth it. I repeat: usually.
The child also scratches his eyes, always and everywhere - at least that is how it looks in clinical practice. Since his immunity at 2–3 years is not as trained as in an adult, it causes various inflammations.
In all other respects, there are no particular differences, but I will still give some tips. If you are not already a child and not yet a parent, then it may still be useful for you. Well, or just interesting.
Washing
The child must wash. Before the age of 1.5–2, this is completely the responsibility of the mother, then in 2-3 years it should be gently reminded that it is worth washing. The child will skip this process, which will increase the risks. You just need to use clean hands a couple of times to splash usual water on your face. Everything. If you are on the road, or if the child is absolutely small, wipe at least with a cotton swab. This is if there are no systemic diseases or different predispositions such as allergies. If there are problems, then medical devices are needed - most often they are antiseptics like furatsilina solution or grandmother’s methods such as chamomile decoction.
Newborns
The most common problem of the smallest, with which we are addressed, is dacryocystitis of newborns. In general, this is an inflammation of the lacrimal sac, in adults (especially in women who love cosmetics), it also happens. But specifically, newborns have a feature. When "initializing" the body systems can be different failures. For example, on the first inhalation, protective films from different tubules should break out. What happens almost always, but not in 100% of cases. If the lacrimal canal remains blocked, a tear cannot leave the eye, and inflammation begins.
The second reason is an infectious process, as a result of which the channel can also be blocked.
In both cases, all this ends with the release of pus. If you start this business, you can lose both eyes. Fortunately, parents respond to all eye diseases of children very quickly. "Launched" are rare, because the child screams confidently. Adults can tolerate, eat painkillers and think that they go to the doctor tomorrow, and the child immediately expresses a life position. And this is very good for our clinical practice.
Treatment of eye inflammation in children is quite simple: purulent crusts and pollution are removed, then broad-spectrum antibiotics are dropped into the eye.
The most interesting place for us here is eye wash. In outpatient clinics, the good old solution of furatsilin is made from his pills, the pus is washed off with antiseptics like chlorhexidine or dear Miramistin. The second option is a decoction of chamomile or calendula (despite the "nationality" of the means, it is a very effective story). Whoever doesn’t know, with chamomile solution even treats the inflammation of the tonsils - they just chase him under pressure on the tonsils, and he cleans and kills everything there.
So here. We in “Geltek” for some similar purposes somehow developed a special sterile napkin. Approximately similar - this was originally the goal was to make a tool for adult resuscitation (and postoperative surgery), and then it began to be used in the nursery. This is a blepharos-naphka like this:
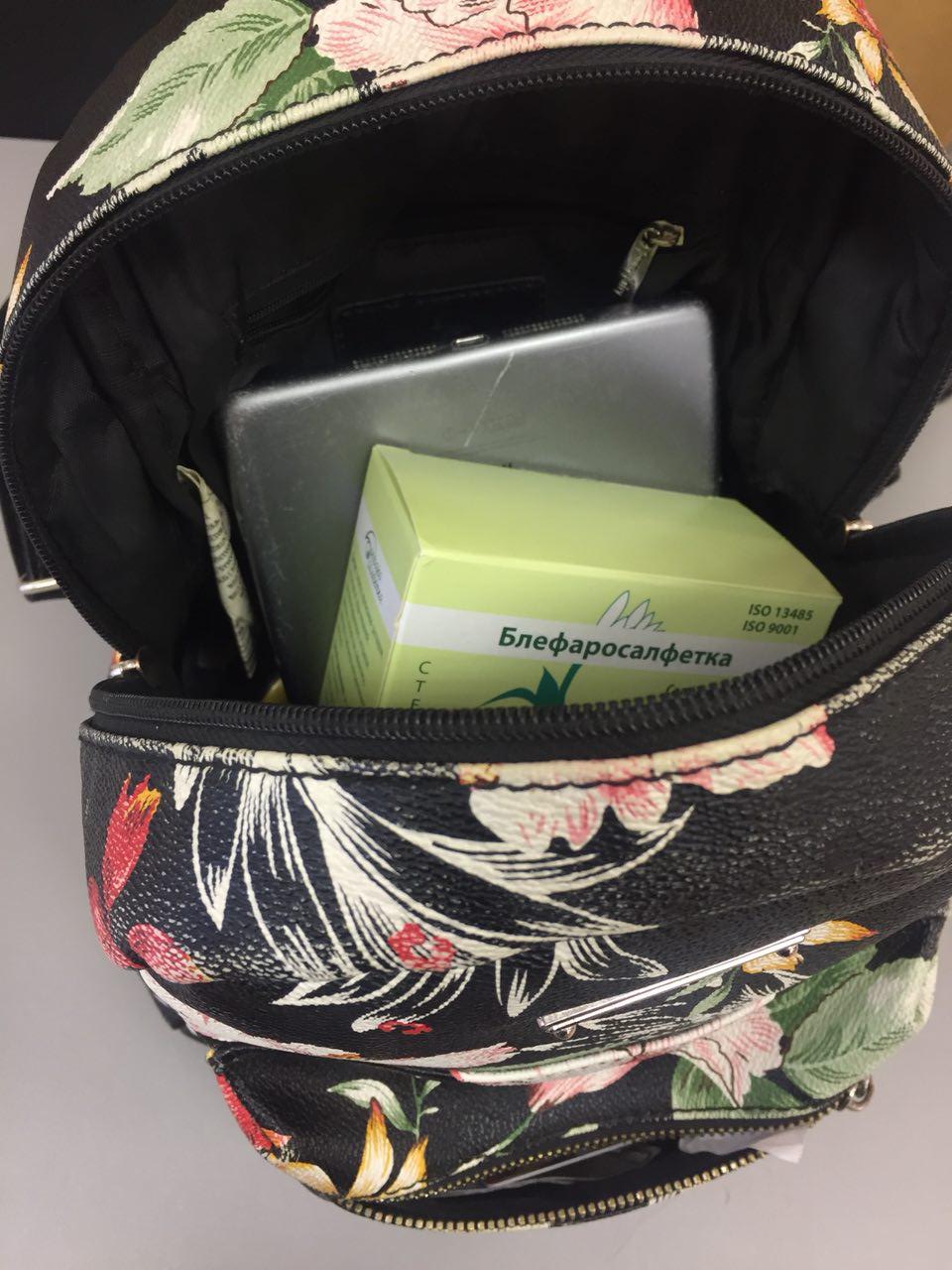
The development has been very successful. A box of 24 pieces of napkins costs 300-400 rubles in a pharmacy, depending on the city, each napkin is in individual foil packaging. I know that patients confidently use them for removing pus in the pediatric treatment. Adults wash her and in the office, and when they go somewhere, many athletes take them for some reason. The only moment is that the ladies for some reason think that she washes away her makeup. Does not wash away, smears. Not for that she.
But back to the child with inflammation of the tear bag. The antibiotic is then dropped and the inner corner of the eye is massaged, where the desired channel passes. If it does not work out mechanically, they make probing. This is not an operation, just passing through a natural channel with a thin metal stick, beating out contamination. Then washed with antiseptic - the same solution furatsilina. If a child does not have congenital deformities of the canal, then the eye ceases to fester.
There is still important to reach the otorhinolaryngologist. Because a nose can grow a polyp or some other problem occurs. The second situation - if there is an underdevelopment of the tear channel or its deformation. In severe cases, create an artificial nasolacrimal canal. Endoscopically get into the nose and drill a hole under general anesthesia. And before that they make an x-ray with contrast (or CT) and a probe trying to get to the level of the lesion.
Kindergarten and school
If a child does not grow in a village, then immunity is difficult to train. Too small sample for training. The horse never sneezed on the mucous membrane, the dog did not lick the eye, the child did not fall into the puddle with manure, and so on. Maybe for the better, but it ends with the fact that when going to kindergarten an active exchange with the microenvironment begins.
Bacterial conjunctivitis appears in all children, without exception. How many are registered on the site - so many will be patients. With time. Sometimes they end easily and quickly without a doctor, but more often parents still try to show it at the first reddening. Peaks come on the first trip to the garden, the first trip to school, the change of class at school and our ophthalmological season - spring and autumn, when children begin to change the microenvironment much more fun.
In case of viral forms, in no case should the eyes be rinsed with tea (tea leaves, tea bags). There is a misconception that it helps. In fact, tea cleans (because the liquid) and reduces sensitivity, but does nothing more. That is, it gives a slight analgesic effect.
In viral keratitis, interferon and other antiviral agents are prescribed, depending on the pathogen, in bacterial histories, a broad spectrum antibiotic. If the inflammation is chronic, then we look at the culture of the medium, the sensitivity of the patient’s bacteria to antibiotics, and also exclude the complex allergic factors. There are rare acanthamous keratitis and extremely rare fungal.
The most frequent case - after the playground, his eyes festered.
Recently, in clinics make it easier. An analysis of the genesis of inflammation (viral or bacterial type) and sensitivity to antibiotics takes 5–7 days (as much as the average culture grows in a Petri dish, to which various types of extermination are then used to evaluate sensitivity). It is also treated for about 7 days. Children with any doubts are prescribed a combination therapy and they take down all opportunistic pathogens from the eyes. Powerful, but far better than waiting. Viral, bacterial, and more exotic species like conjunctivitis, keratitis, and dacryocystitis often differ in appearance, and a doctor with a couple of years of practice with children can determine what it is, visually. Doubt - combination therapy.
Fungi, or rather spores, usually cause allergic reactions, but not directly fungal. The only exception is children with very weak immunity, usually after several courses of antibiotics. I personally had only one such case in practice.
In second place at this age - allergies. Everything is clear there. Allergen is detected and eliminated. Unfortunately, this possibility is not always the case, then general desensitization therapy is carried out. Allergies can be from a heap of reasons, including interesting mixed ones. For example, I had a patient with allergies to the fur of small mammals (dogs, cats, mice, guinea pigs), citrus, and fungi. Parents are very conscious, in time led.
Minor injuries
These are injuries like “a branch flew in” or “ran along the street, caught a grain of sand in the eye”. If the child complains after washing with water - you need to check. If something is left, it can get under the upper eyelid and irritate wildly from there, scratching the cornea. There was a recent case - a young girl came. Her glitter from the shadows fell under the eyelid.
We must look and get it. It is better to do the doctor on small objects, and large ones there do not particularly get stuck (except for cases of severe penetrating wounds of the eye, but this is not to be addressed to the clinic, but to specialized departments where there is microsurgery). In field conditions, most often ordinary clean water helps. If there is no water, any eye drops, but here chlorhexidine or vasoconstrictor with anesthetics is not necessary.
A small child can buy glasses with frames made from bending polymer (for example, silicone), they are on average more expensive and create a little more aberrations, but you can not be afraid that he will break them, and then you can get it all out of your eye.
Other
The remaining processes are not very different from adult ophthalmology. There are features in resuscitation, with which I work, but in everyday life it usually does not manifest in any way. Next time, I’ll still get to the topic of what carpets do with sight, and generally tell you about what can be changed in the apartment. This all applies to children.
And, still there are children's shampoos to wash your hair without tears, if they fall into the eye. There are no active substances that cause irritation of the mucous membranes, just mild agents (as a rule, more expensive and a little worse than cleaning products). But still, it’s impossible to follow his instructions in the eyes, that is, if he gets caught, he willn’t pinch, but the eye doesn’t care and it may become worse. But in practice only because of the shampoo there were no appeals.
Source: https://habr.com/ru/post/410019/