Anesthesia in modern oncology
Pain syndrome in cancer occurs in 35-50% of patients in the early stages of the malignant process. As the disease progresses, up to 80% already feel moderate to severe pain. In the terminal stage, it hurts almost everyone - 95% of patients. Pain interferes with sleep, eating, moving, making informed decisions, affecting the work of organs and systems.
The good news is that modern medicine has learned to control this pain in 90% of cases. That is, either to stop pain syndrome completely, or to significantly reduce its intensity. Thus, at any stage of cancer, it is possible to maintain normal quality of life for cancer patients.
We have already written that in Medicine 24/7, more than half of the patients are from stage III-IV of cancer. The first thing you have to do when providing palliative care to such people is the relief of pain. Therefore, adequate anesthesia for our profile remains one of the most relevant areas of work.
In Russia, there are specific problems associated with obtaining analgesics, especially narcotic, and with non-compliance in some medical institutions with the WHO recommendations for anesthesia.
Although, judging by our practice, the basic principle is quite simple: “Do not make sharp movements.” Always start with minimal doses, increase the power of pain relief very smoothly, and not jump from ordinary ibuprofen directly to morphine, “taking away” a lot of alternative weaker options from the patient that could be used for a long time.
Today we will try to figure out what kind of medicine is needed for whom and when, and how else modern medicine can deal with pain.
And for what kind of sins does nature torment people? The official definition of the IASP (International Association for the Study of Pain) is: "Pain is an unpleasant sensory or emotional experience associated with actual or potential tissue damage, or described in terms of such damage . " Translate to the human.
Normally, pain is an important and useful thing for survival. This is a clear signal to the brain from some part of the body or from an internal organ: “Hey, pay attention, there are serious problems, something needs to be done. Quickly!". This signal system allows a person to avoid too serious injuries and damages: if you feel unpleasant, you will try not to interact further with the cause of your troubles. So, you are more likely to remain safe and almost unharmed. So everything happened in the course of evolution.

Reflex withdrawal - a healthy biological response to acute pain
But in an unhealthy body of an oncological patient (as well as a patient with a cardiovascular disease or HIV, or, for example, tuberculosis), pain loses its useful signaling function and vice versa, interferes with both primary therapy and the provision of palliative care. The patient falls into a depressive state, losing the strength necessary to combat the disease. Chronic pain syndrome turns into an independent pathology, which must be separately treated.
That is why more than a million people in Russia need pain relief every year. Moreover, from 400 to 800 thousand of them (according to various estimates) need opioid analgesics.
To figure out what approach is needed to relieve pain, the oncologist needs to understand its cause and origin.
One of the great difficulties in diagnosing ZNO (malignant neoplasms) is that the patient often doesn’t have any pain at all. The tumor is corny may still be too small.
This also happens if the tumor grows in loose tissues (such as the mammary gland) or grows inside the organ cavity (for example, the stomach). Also without pain, those types of cancer can develop that do not have solid primary tumors - leukemias, malignant diseases of the hematopoietic system.
In our practice, there have been cases when even stage IV of oncological processes proceeded asymptomatically — until the appearance of multiple metastases, the patient did not suffer.
In all other cases, when the pain is present, it is important for the doctor to know what caused it. For reasons of occurrence, we distinguish three main groups.
Additional complicating "bonuses" to the main types of cancer pain add painful manifestations of side effects from the antitumor therapy itself:
Modern doctors use more and more accurately dosed radiation therapy, more and more “accurate”, targeted drugs, less and less traumatic surgery to reduce the frequency and severity of such unpleasant side effects. Today, in the clinic, for example, we perform much more surgical interventions with endoscopic and laparoscopic methods - through thin punctures or very small (1-1.5 cm) incisions in the skin. Methods are all the same: to prolong the patient's normal life.
To choose adequate analgesia, the doctor must understand how painful it is to the person, try to understand exactly where it hurts and for how long. The prescription for anesthesia depends on this. In addition to clarifying questions about the nature and location of pain, the doctor necessarily assesses its intensity.
All over the world, NOSH scales (numerological rating scale) and VAS (visual analogue scale), or hybrid variants, depending on the age and condition of the patient, are used for this. For very young children and very elderly people, as well as for patients with cognitive impairment, it can be difficult to answer standard questions. Sometimes you have to work with such only on behavior and facial expressions.

The scale of assessment of pain from 0 (nothing hurts) to 10 (unbearably painful)
It is important to get as much additional information as possible: if the patient believes that tolerating is a worthy occupation, and complaining is unworthy, or it turns out that the patient had periods of abuse and addictions, this can make adjustments to pain therapy.
We have already touched upon the topic of working with the psychological state of the patient, and we will touch it once more - it is important to remember this both for the doctors and the relatives of the patient. WHO even introduced a special concept for this: total pain. It covers not only physical stimuli, but also emotional and social negative aspects of a patient’s life.

The pain of a cancer patient is much deeper and more complicated than it seems from the outside. Pain therapy is a case where the physician must treat the patient's subjective assessments with special attention.
Considering such a multicomponent pool of reasons for increasing pain, the world medical community recognizes the most successful idea of “multimodal” therapy - when along with drug treatment, physical activity is applied by the patient, relaxation techniques and psychotherapy. All this creates conditions under which pain ceases to occupy a central place in the patient's life, giving way to more important and interesting areas.
Probably, every doctor considers as more correct and successful those drugs that turned out to be the most effective in his personal practical experience. But any oncologist, trying to stop pain, should remember the WHO recommendations for the treatment of cancer pain.
These recommendations were built in the form of a three-step "ladder" in 1986, and since then the basic tenets have remained unchanged.
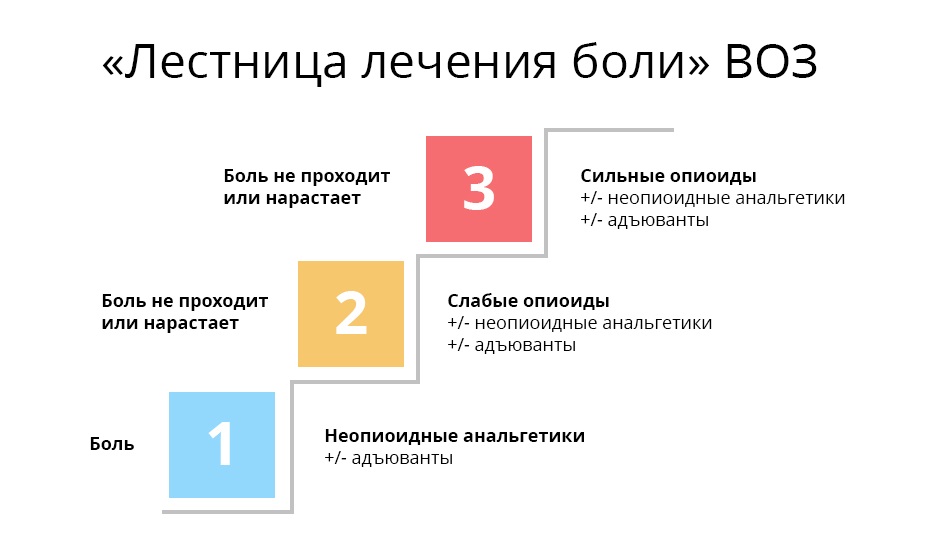
First stage. With mild pain, begin with non-narcotic analgesics and nonsteroidal anti-inflammatory drugs and drugs (NSAIDs / NSAIDs). These are the usual OTC paracetamol, ibuprofen, aspirin, and others. Diclofenac and others are prescribed for muscle and joint pain.

The scheme of action of NSAIDs - they block the enzyme cyclooxygenase, reducing the synthesis of prostaglandins, thereby reducing the sensitivity of pain receptors.
Such drugs are not addictive and addictive, but in a large dosage can harm the gastrointestinal tract, therefore, infinitely and uncontrollably, the dose cannot be increased, so as not to complicate the situation with gastric bleeding.
The second step. Further, if the pain intensifies, codeine and tramadol are prescribed. These are "light" opiates. They act by attaching to the opioid receptors of the central nervous system and replacing endorphins there.
Endorphins are neurotransmitters, one of the functions of which is to inhibit the transmission of weak pain impulses from the spinal cord to the head. This allows us not to cry of pain every time we put our elbows on the table or jump from a height of half a meter. But with intense pain, endorphin production decreases. Opioid receptors are released, nerve impulses are not inhibited, the person is in pain.
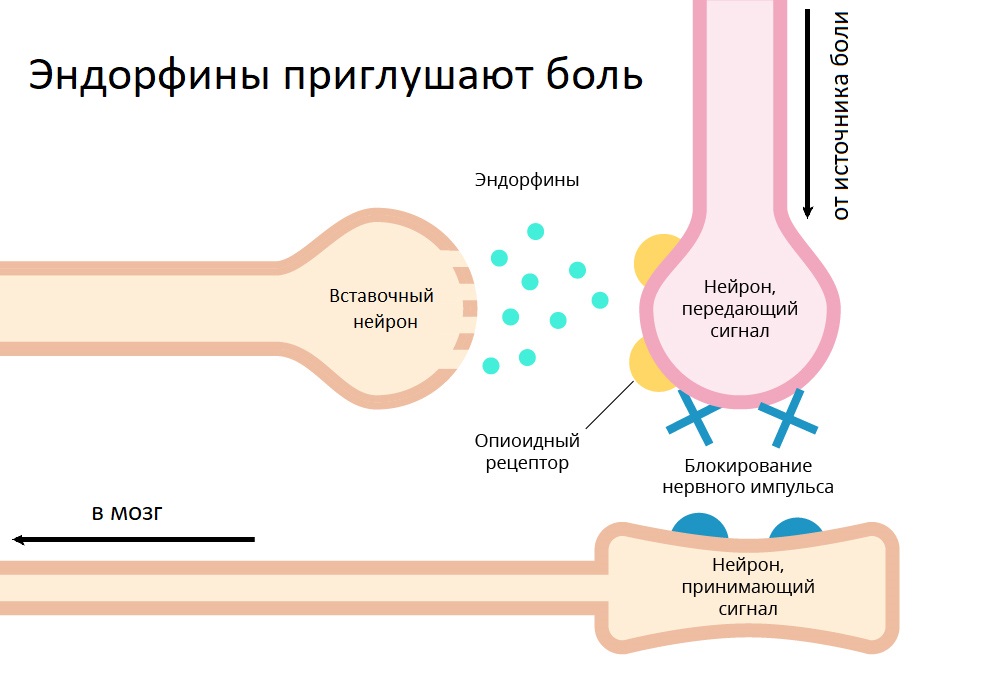
This is how a braking intercalary neuron usually behaves - it releases endorphins to block the incoming nerve impulses so that the brain “doesn’t pay attention”
Tramadol is taken together with analgin, paracetamol and other first-stage drugs - the effect is complex: simultaneous effects on the central and peripheral nervous system.
It is important that tramadol, although it is an opiate, refers to non-narcotic analgesics. The patient is easier to get it and do not need to be afraid of potential dependence.
The third step. The doctor and his patient end up at this stage when weak opiates have stopped helping him. Strong opiates come into play, the main one is morphine. Strong opiates bind to opioid receptors much more reliably than weak ones, therefore they act more potently. However, this effect is expensive: these drugs can already cause addiction - but only if they are used incorrectly and uncontrollably.
Therefore, the third step is beginning to climb as gradually. Buprenorphine or fentanyl is prescribed, the effectiveness of which is 50% and 75% relative to morphine - and they are administered strictly on schedule, starting from the minimum dose. Under the supervision of a physician, subject to the recommended dosages and frequency of administration, with a gradual increase in “power”, the likelihood of developing pathological dependence is extremely small.
It is important that the so-called adjuvant, that is, auxiliary, therapy can be used at each stage. Adjuvant drugs do not anesthetize themselves, but in combination with the main analgesics either enhance their effect, or level side effects. This group includes antidepressants, corticosteroids, antiemetic and anticonvulsant, antihistamine, etc.
Thus, WHO provides the basic principles and recommendations for a smooth transition from step to step, which help to avoid a deadlock in therapy - when the pain intensifies, and the means to combat it no longer exists.
This happens if the oncologist prescribes opioid drugs ahead of time or at a dose of more than necessary. If you jump from ketorol to promedol (as, unfortunately, some doctors do - some due to inexperience, some due to the lack of the necessary drugs), then the effect can first exceed the expectations. But then it turns out that the pain will require an increase in dosage faster than prescribed by a safe regimen. The steps will end before you take the required number of steps. In this case, the doctor himself takes away the means of treatment.
From the patient’s side, the main one is awesome! - A mistake is to “endure to the end.” Especially in Russian patients, it is noticeable. When they come to us for treatment from the Baltic states, for example, they no longer have this superfluous partisan "heroism".
And rightly so - talk to the doctor about the pain immediately. Because in the treatment of pain there is one unpleasant paradox: the longer you endure, the harder it is to get rid of pain. The fact is that prolonged long pain means prolonged and persistent excitation of the same conductive nerve pathways. Nociogenic nerve cells, say, “get used” to conduct pain impulses and their sensitization occurs - an increase in sensitivity. In the future, they easily respond with a painful response even to weak and harmless effects. With such pain it becomes much harder to cope.
Strictly speaking, just injections, that is to say injections, in modern anesthesia they try not to use. To choose for pain relief the most painful method of administration is somehow illogical.
Therefore, nowadays, the Transdermal Method of Introduction is becoming more popular.
Unlike injections, it is the most convenient for the patient. He has his limitations, of course - in body temperature, in the amount of subcutaneous fat, but in most cases it is good:

Fentanyl plaster - strong, safe and comfortable pain relief
Medical blockade of nerves and vegetative plexuses. Anesthetic, a drug for “freezing,” is injected directly into the site of nerve projection, through which pain from a cancer organ is transmitted. Depending on the type of anesthetic and nosology (type of tumor), this is done with a different frequency - from once a week to once every 6 months. The method is widely distributed, because it has almost no contraindications.
Spinal anesthesia. The drug (morphine, fentanyl) is injected into the spinal canal, where the spinal cord lies. Through the cerebrospinal fluid and with the bloodstream, the drug enters the brain and "turns off" the sensitivity, the muscles relax. The method is used for very acute and intense pain.
Epidural anesthesia. Yes, it is made not only pregnant. The same drugs that, with spinal anesthesia, are injected into the cavity between the dura mater and the walls of the spinal canal. Epidural anesthesia is used in the later stages, with metastatic bone lesions, when the pain is not relieved by injections and oral preparations.
Palliative chemo, targeted and radiation therapy. It is not used for the purpose of destroying a tumor, but with the goal of simply making it smaller, in order to release the squeezed nerve glands causing pain.
Neurosurgical methods. The neurosurgeon cuts the roots of the spinal or cranial nerves. This does not lead to the loss of motor activity (although it may require rehabilitation), but the brain is deprived of the opportunity to receive pain signals along this path.
Radiofrequency ablation (RFA). In our first post, on palliative medicine , we attached a video about how this method helped the patient to get rid of pain at the last stage of cancer. At that time, RFA was used to destroy metastases that pressed on the nerve roots of the spinal cord.
In cases where it is impossible to destroy metastases or the tumor itself, RFA can be used to destroy the conductive nerve pathways. This is similar to the previous version, only the surgeon does not act with a scalpel, but with a special needle heated by radiofrequency oscillations to a high temperature.
Neurolysis with endosonography. Neurolysis is the destruction of the nerve pathway conducting pain with the help of special chemical solutions. Under the control of ultrasound, the endoscope is brought exactly to the celiac (solar) nerve plexus through the gastrointestinal tract and destroy part of the nerve fibers. The analgesic effect of the procedure occurs in 90% of cases with stomach cancer or, for example, pancreas. The result of the procedure is preserved from a month to a year in rare cases. It all depends on the speed of development of the tumor. Given that in the case of the use of drugs, analgesics, they would have to apply weekly.
Vertebroplasty. This method can be explained by a live example from our own practice. Damage to the spinal column by metastases leads to the destruction of the vertebral body. The bone structure of the vertebra is deformed, compression occurs (squeezing) of the spinal roots. Occurs radicular compression cider, which is accompanied by severe pain. Vertebroplasty strengthens the body of the affected vertebra so that it ceases to press on the nerve roots.
The operation is minimally invasive, it is performed under local anesthesia and control of computed tomography. A special cannula needle is inserted into the vertebral body, while the height of the vertebra is restored by the special instruments. Bone cement is introduced into the vertebral cavity. The result of the intervention is also monitored by a CT scan. In 98% of cases, vertebroplasty eliminates pain immediately after the end of the operation. The rehabilitation period is minimal, after a couple of hours the patient can assume a vertical position.
So, a good oncologist has many options to help a patient with pain syndrome today. We are convinced that regardless of the stage of his cancer, a person can have a normal quality of life for as long as possible, without restrictions and suffering.
The problem of insufficient provision of strong analgesics for patients with severe diagnoses is one of the most, sorry, patient problems in Russian oncology in particular, and palliative medicine in general.
Yes, you will say that we have all these processes in a private clinic, patients and their families do not have to spend weeks trying to get the necessary stamp on the prescription from the doctor and then regain the free packaging of the drug from the pharmacy. But our doctors for many years worked in public hospitals, we receive patients every week who have just come from there, so the gravity of the situation is clear to us.
After the suicide of Rear Admiral Apanasenko in 2014, some progress began, but not everything is as rosy as promised.
Many doctors simply do not want to prescribe drugs from the group of narcotic analgesics (and we remember, only they help at level 3) because they are afraid. Everyone remembers the resonant case of Alevtina Khorinyak . She was fully acquitted, but many are also afraid to go on trial for alleged "illegal traffic."
Patients, in turn, are afraid to take tramadol, considering it something similar to heroin. Hopefully, the part of the article where we explain about the "ladder" of WHO - a little streamlined this information in the heads of citizens.
So that there is no more fear, and therefore no potential unnecessary pain, let us explain what procedure is necessary to obtain a narcotic drug.
Who writes the recipe?
How long does the recipe work?
15 days. Enough for any "holidays". But if he is needed urgently, then he can be discharged both on a holiday and on a holiday.
Do I need to take ampoules?
Not. By law, no one has the right to require the patient or his family to donate used ampoules, patches and packaging from narcotic analgesics.
Can one of the relatives get a prescription and a drug on behalf of the patient?
What should I do if I am having difficulty getting an anesthetic?
In conclusion, I want to somehow summarize everything said on this difficult topic:
Let nothing else hurt you for a very, very long time!
The good news is that modern medicine has learned to control this pain in 90% of cases. That is, either to stop pain syndrome completely, or to significantly reduce its intensity. Thus, at any stage of cancer, it is possible to maintain normal quality of life for cancer patients.
We have already written that in Medicine 24/7, more than half of the patients are from stage III-IV of cancer. The first thing you have to do when providing palliative care to such people is the relief of pain. Therefore, adequate anesthesia for our profile remains one of the most relevant areas of work.
In Russia, there are specific problems associated with obtaining analgesics, especially narcotic, and with non-compliance in some medical institutions with the WHO recommendations for anesthesia.
Although, judging by our practice, the basic principle is quite simple: “Do not make sharp movements.” Always start with minimal doses, increase the power of pain relief very smoothly, and not jump from ordinary ibuprofen directly to morphine, “taking away” a lot of alternative weaker options from the patient that could be used for a long time.
Today we will try to figure out what kind of medicine is needed for whom and when, and how else modern medicine can deal with pain.
What is pain in general?
And for what kind of sins does nature torment people? The official definition of the IASP (International Association for the Study of Pain) is: "Pain is an unpleasant sensory or emotional experience associated with actual or potential tissue damage, or described in terms of such damage . " Translate to the human.
Normally, pain is an important and useful thing for survival. This is a clear signal to the brain from some part of the body or from an internal organ: “Hey, pay attention, there are serious problems, something needs to be done. Quickly!". This signal system allows a person to avoid too serious injuries and damages: if you feel unpleasant, you will try not to interact further with the cause of your troubles. So, you are more likely to remain safe and almost unharmed. So everything happened in the course of evolution.

Reflex withdrawal - a healthy biological response to acute pain
But in an unhealthy body of an oncological patient (as well as a patient with a cardiovascular disease or HIV, or, for example, tuberculosis), pain loses its useful signaling function and vice versa, interferes with both primary therapy and the provision of palliative care. The patient falls into a depressive state, losing the strength necessary to combat the disease. Chronic pain syndrome turns into an independent pathology, which must be separately treated.
That is why more than a million people in Russia need pain relief every year. Moreover, from 400 to 800 thousand of them (according to various estimates) need opioid analgesics.
What and why hurt cancer?
To figure out what approach is needed to relieve pain, the oncologist needs to understand its cause and origin.
One of the great difficulties in diagnosing ZNO (malignant neoplasms) is that the patient often doesn’t have any pain at all. The tumor is corny may still be too small.
This also happens if the tumor grows in loose tissues (such as the mammary gland) or grows inside the organ cavity (for example, the stomach). Also without pain, those types of cancer can develop that do not have solid primary tumors - leukemias, malignant diseases of the hematopoietic system.
In our practice, there have been cases when even stage IV of oncological processes proceeded asymptomatically — until the appearance of multiple metastases, the patient did not suffer.
In all other cases, when the pain is present, it is important for the doctor to know what caused it. For reasons of occurrence, we distinguish three main groups.
- Nociceptive pain. Awakened by nociceptors - pain receptors. These receptors are a network of branched peripheral nerve endings that “connect” to the spinal cord all our internal organs, as well as bones, and each point on the surface of the skin. When damage (or exposure that threatens to damage) of any part of the body, the nociceptors send a signal to the spinal cord, which, firstly, triggers avoidance reflexes (for example, jerk the hand off during a burn), and secondly, “reports upwards” - in brain.
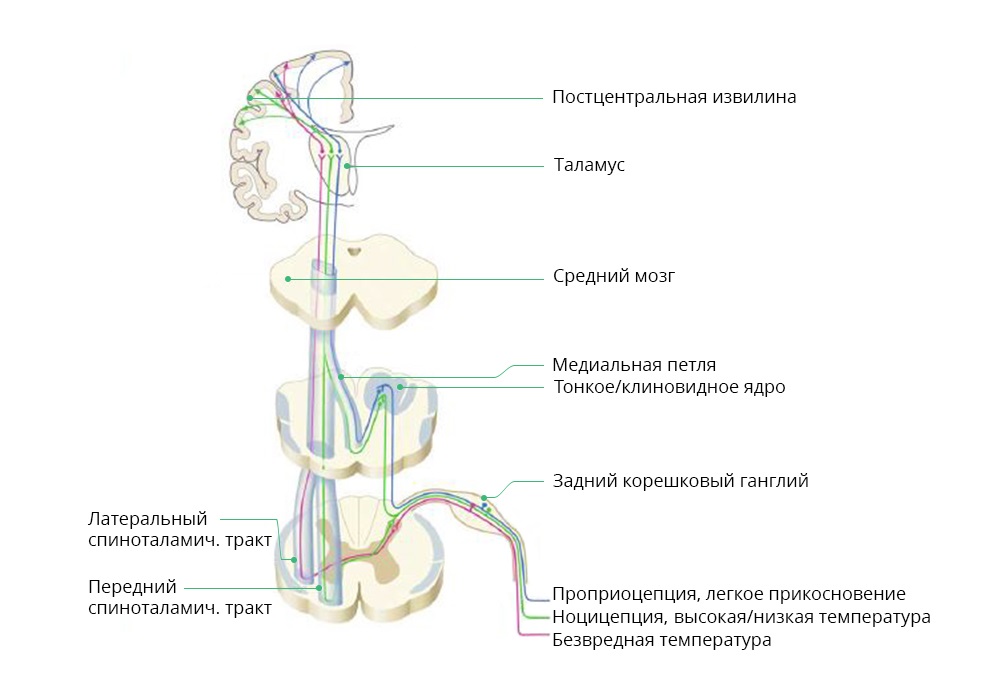
The scheme of passage of nociceptive and other signals from external stimuli
And there the complex interaction of the thalamus, hypothalamus and cerebral cortex triggers stress reactions of the autonomic nervous system: dilated pupils, increased pulse, increased pressure, etc. At some point, the brain “suspends” all other nervous processes, because pain has first priority. It is more important than anything else for survival - the brain considers. And the patient at this moment can not normally think and do some other things.
In oncological diseases, nociceptive pain is most often a reaction to the tumor itself or metastasis. Thus, metastases in the spine can give a breakthrough, sharp pain when the patient changes the position of the body. - Neuropathic pain. Its reason - a violation of the nerve structures - nerves, spinal cord or brain. Combines two factors: on the one hand, the intensity - the patient is very painful, sometimes even potent analgesics do not help. On the other hand, localization is difficult. Unlike acute nociceptive pain, the patient often cannot tell exactly where he is in pain.
Such pain is caused by the growth of a tumor or metastasis, when they press, for example, on the spine or pinch the nerve roots. Also the cause, unfortunately, can be the side effects of anticancer treatment. - Dysfunctional pain. The case when the organic causes of pain are absent, but it does not go away: for example, the tumor has already been removed, the healing after the surgery has passed, and the pain has remained. It happens that the pain, according to the patient himself, is much stronger than it should be in his state of health.
In such cases, it is necessary to take into account the psychological state of the patient. Strong stress can significantly affect perception changes, even to completely psychogenic pain.
Our clinical practice shows how strongly knowledge of onco-psychology helps in such cases. In Russia, not all doctors pay due attention to it, although it is in this situation that it helps to stabilize the patient’s condition and reduce his painful pain syndrome.
Additional complicating "bonuses" to the main types of cancer pain add painful manifestations of side effects from the antitumor therapy itself:
- pain during healing after operations;
- cramps and cramps;
- ulceration of mucous membranes;
- joint and muscle pain;
- skin inflammation, dermatitis.
Modern doctors use more and more accurately dosed radiation therapy, more and more “accurate”, targeted drugs, less and less traumatic surgery to reduce the frequency and severity of such unpleasant side effects. Today, in the clinic, for example, we perform much more surgical interventions with endoscopic and laparoscopic methods - through thin punctures or very small (1-1.5 cm) incisions in the skin. Methods are all the same: to prolong the patient's normal life.
How much pain, in points?
To choose adequate analgesia, the doctor must understand how painful it is to the person, try to understand exactly where it hurts and for how long. The prescription for anesthesia depends on this. In addition to clarifying questions about the nature and location of pain, the doctor necessarily assesses its intensity.
All over the world, NOSH scales (numerological rating scale) and VAS (visual analogue scale), or hybrid variants, depending on the age and condition of the patient, are used for this. For very young children and very elderly people, as well as for patients with cognitive impairment, it can be difficult to answer standard questions. Sometimes you have to work with such only on behavior and facial expressions.

The scale of assessment of pain from 0 (nothing hurts) to 10 (unbearably painful)
It is important to get as much additional information as possible: if the patient believes that tolerating is a worthy occupation, and complaining is unworthy, or it turns out that the patient had periods of abuse and addictions, this can make adjustments to pain therapy.
We have already touched upon the topic of working with the psychological state of the patient, and we will touch it once more - it is important to remember this both for the doctors and the relatives of the patient. WHO even introduced a special concept for this: total pain. It covers not only physical stimuli, but also emotional and social negative aspects of a patient’s life.

The pain of a cancer patient is much deeper and more complicated than it seems from the outside. Pain therapy is a case where the physician must treat the patient's subjective assessments with special attention.
Considering such a multicomponent pool of reasons for increasing pain, the world medical community recognizes the most successful idea of “multimodal” therapy - when along with drug treatment, physical activity is applied by the patient, relaxation techniques and psychotherapy. All this creates conditions under which pain ceases to occupy a central place in the patient's life, giving way to more important and interesting areas.
What is the treatment for cancer pain, or where does the anesthesia lead?
Probably, every doctor considers as more correct and successful those drugs that turned out to be the most effective in his personal practical experience. But any oncologist, trying to stop pain, should remember the WHO recommendations for the treatment of cancer pain.
These recommendations were built in the form of a three-step "ladder" in 1986, and since then the basic tenets have remained unchanged.
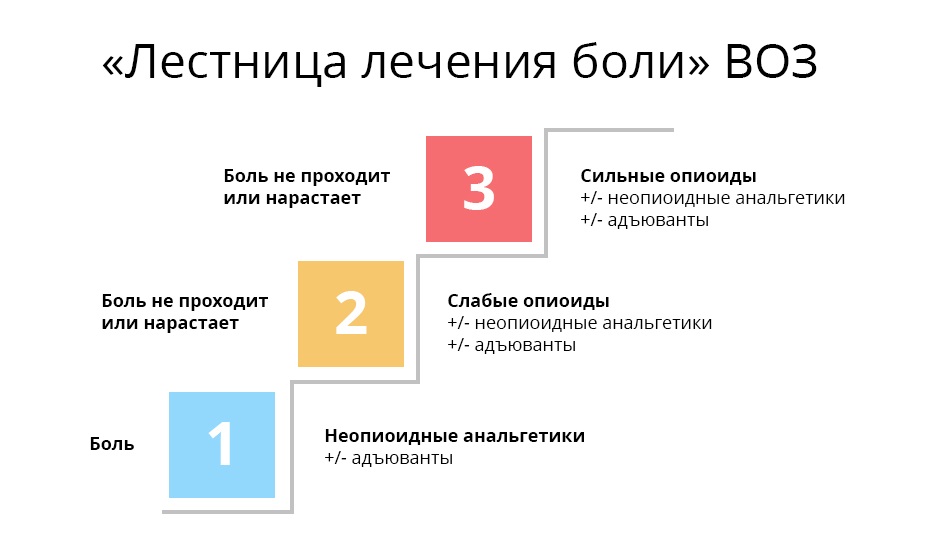
First stage. With mild pain, begin with non-narcotic analgesics and nonsteroidal anti-inflammatory drugs and drugs (NSAIDs / NSAIDs). These are the usual OTC paracetamol, ibuprofen, aspirin, and others. Diclofenac and others are prescribed for muscle and joint pain.

The scheme of action of NSAIDs - they block the enzyme cyclooxygenase, reducing the synthesis of prostaglandins, thereby reducing the sensitivity of pain receptors.
Such drugs are not addictive and addictive, but in a large dosage can harm the gastrointestinal tract, therefore, infinitely and uncontrollably, the dose cannot be increased, so as not to complicate the situation with gastric bleeding.
The second step. Further, if the pain intensifies, codeine and tramadol are prescribed. These are "light" opiates. They act by attaching to the opioid receptors of the central nervous system and replacing endorphins there.
Endorphins are neurotransmitters, one of the functions of which is to inhibit the transmission of weak pain impulses from the spinal cord to the head. This allows us not to cry of pain every time we put our elbows on the table or jump from a height of half a meter. But with intense pain, endorphin production decreases. Opioid receptors are released, nerve impulses are not inhibited, the person is in pain.
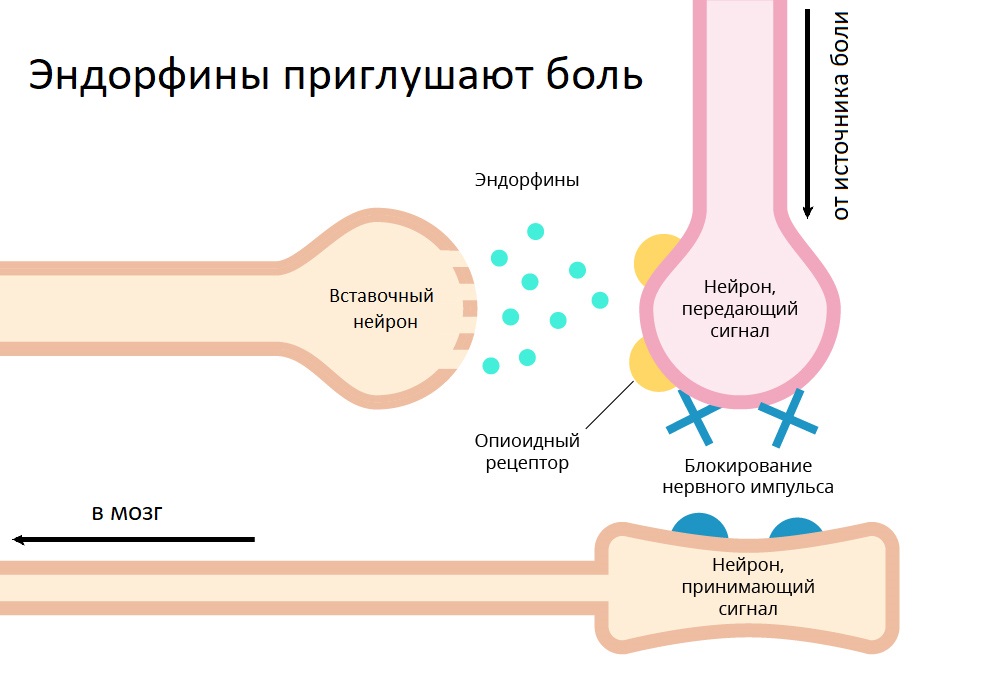
This is how a braking intercalary neuron usually behaves - it releases endorphins to block the incoming nerve impulses so that the brain “doesn’t pay attention”
Tramadol is taken together with analgin, paracetamol and other first-stage drugs - the effect is complex: simultaneous effects on the central and peripheral nervous system.
It is important that tramadol, although it is an opiate, refers to non-narcotic analgesics. The patient is easier to get it and do not need to be afraid of potential dependence.
The third step. The doctor and his patient end up at this stage when weak opiates have stopped helping him. Strong opiates come into play, the main one is morphine. Strong opiates bind to opioid receptors much more reliably than weak ones, therefore they act more potently. However, this effect is expensive: these drugs can already cause addiction - but only if they are used incorrectly and uncontrollably.
Therefore, the third step is beginning to climb as gradually. Buprenorphine or fentanyl is prescribed, the effectiveness of which is 50% and 75% relative to morphine - and they are administered strictly on schedule, starting from the minimum dose. Under the supervision of a physician, subject to the recommended dosages and frequency of administration, with a gradual increase in “power”, the likelihood of developing pathological dependence is extremely small.
It is important that the so-called adjuvant, that is, auxiliary, therapy can be used at each stage. Adjuvant drugs do not anesthetize themselves, but in combination with the main analgesics either enhance their effect, or level side effects. This group includes antidepressants, corticosteroids, antiemetic and anticonvulsant, antihistamine, etc.
Why is it important to follow the recommendations and principles of WHO?
Thus, WHO provides the basic principles and recommendations for a smooth transition from step to step, which help to avoid a deadlock in therapy - when the pain intensifies, and the means to combat it no longer exists.
This happens if the oncologist prescribes opioid drugs ahead of time or at a dose of more than necessary. If you jump from ketorol to promedol (as, unfortunately, some doctors do - some due to inexperience, some due to the lack of the necessary drugs), then the effect can first exceed the expectations. But then it turns out that the pain will require an increase in dosage faster than prescribed by a safe regimen. The steps will end before you take the required number of steps. In this case, the doctor himself takes away the means of treatment.
From the patient’s side, the main one is awesome! - A mistake is to “endure to the end.” Especially in Russian patients, it is noticeable. When they come to us for treatment from the Baltic states, for example, they no longer have this superfluous partisan "heroism".
And rightly so - talk to the doctor about the pain immediately. Because in the treatment of pain there is one unpleasant paradox: the longer you endure, the harder it is to get rid of pain. The fact is that prolonged long pain means prolonged and persistent excitation of the same conductive nerve pathways. Nociogenic nerve cells, say, “get used” to conduct pain impulses and their sensitization occurs - an increase in sensitivity. In the future, they easily respond with a painful response even to weak and harmless effects. With such pain it becomes much harder to cope.
What besides the shots?
Strictly speaking, just injections, that is to say injections, in modern anesthesia they try not to use. To choose for pain relief the most painful method of administration is somehow illogical.
Therefore, nowadays, the Transdermal Method of Introduction is becoming more popular.
Unlike injections, it is the most convenient for the patient. He has his limitations, of course - in body temperature, in the amount of subcutaneous fat, but in most cases it is good:
- the drug (usually fentanyl) is released gradually, lasts for 72 hours;
- does not require monitoring the time of taking the pills or the introduction of drugs;
- eliminates overdose (this is important for a narcotic analgesic).

Fentanyl plaster - strong, safe and comfortable pain relief
Medical blockade of nerves and vegetative plexuses. Anesthetic, a drug for “freezing,” is injected directly into the site of nerve projection, through which pain from a cancer organ is transmitted. Depending on the type of anesthetic and nosology (type of tumor), this is done with a different frequency - from once a week to once every 6 months. The method is widely distributed, because it has almost no contraindications.
Spinal anesthesia. The drug (morphine, fentanyl) is injected into the spinal canal, where the spinal cord lies. Through the cerebrospinal fluid and with the bloodstream, the drug enters the brain and "turns off" the sensitivity, the muscles relax. The method is used for very acute and intense pain.
Epidural anesthesia. Yes, it is made not only pregnant. The same drugs that, with spinal anesthesia, are injected into the cavity between the dura mater and the walls of the spinal canal. Epidural anesthesia is used in the later stages, with metastatic bone lesions, when the pain is not relieved by injections and oral preparations.
Palliative chemo, targeted and radiation therapy. It is not used for the purpose of destroying a tumor, but with the goal of simply making it smaller, in order to release the squeezed nerve glands causing pain.
Neurosurgical methods. The neurosurgeon cuts the roots of the spinal or cranial nerves. This does not lead to the loss of motor activity (although it may require rehabilitation), but the brain is deprived of the opportunity to receive pain signals along this path.
Radiofrequency ablation (RFA). In our first post, on palliative medicine , we attached a video about how this method helped the patient to get rid of pain at the last stage of cancer. At that time, RFA was used to destroy metastases that pressed on the nerve roots of the spinal cord.
In cases where it is impossible to destroy metastases or the tumor itself, RFA can be used to destroy the conductive nerve pathways. This is similar to the previous version, only the surgeon does not act with a scalpel, but with a special needle heated by radiofrequency oscillations to a high temperature.
Neurolysis with endosonography. Neurolysis is the destruction of the nerve pathway conducting pain with the help of special chemical solutions. Under the control of ultrasound, the endoscope is brought exactly to the celiac (solar) nerve plexus through the gastrointestinal tract and destroy part of the nerve fibers. The analgesic effect of the procedure occurs in 90% of cases with stomach cancer or, for example, pancreas. The result of the procedure is preserved from a month to a year in rare cases. It all depends on the speed of development of the tumor. Given that in the case of the use of drugs, analgesics, they would have to apply weekly.
Vertebroplasty. This method can be explained by a live example from our own practice. Damage to the spinal column by metastases leads to the destruction of the vertebral body. The bone structure of the vertebra is deformed, compression occurs (squeezing) of the spinal roots. Occurs radicular compression cider, which is accompanied by severe pain. Vertebroplasty strengthens the body of the affected vertebra so that it ceases to press on the nerve roots.
The operation is minimally invasive, it is performed under local anesthesia and control of computed tomography. A special cannula needle is inserted into the vertebral body, while the height of the vertebra is restored by the special instruments. Bone cement is introduced into the vertebral cavity. The result of the intervention is also monitored by a CT scan. In 98% of cases, vertebroplasty eliminates pain immediately after the end of the operation. The rehabilitation period is minimal, after a couple of hours the patient can assume a vertical position.
So, a good oncologist has many options to help a patient with pain syndrome today. We are convinced that regardless of the stage of his cancer, a person can have a normal quality of life for as long as possible, without restrictions and suffering.
The main pain is the imperfection of the system
The problem of insufficient provision of strong analgesics for patients with severe diagnoses is one of the most, sorry, patient problems in Russian oncology in particular, and palliative medicine in general.
Yes, you will say that we have all these processes in a private clinic, patients and their families do not have to spend weeks trying to get the necessary stamp on the prescription from the doctor and then regain the free packaging of the drug from the pharmacy. But our doctors for many years worked in public hospitals, we receive patients every week who have just come from there, so the gravity of the situation is clear to us.
After the suicide of Rear Admiral Apanasenko in 2014, some progress began, but not everything is as rosy as promised.
Many doctors simply do not want to prescribe drugs from the group of narcotic analgesics (and we remember, only they help at level 3) because they are afraid. Everyone remembers the resonant case of Alevtina Khorinyak . She was fully acquitted, but many are also afraid to go on trial for alleged "illegal traffic."
Patients, in turn, are afraid to take tramadol, considering it something similar to heroin. Hopefully, the part of the article where we explain about the "ladder" of WHO - a little streamlined this information in the heads of citizens.
So that there is no more fear, and therefore no potential unnecessary pain, let us explain what procedure is necessary to obtain a narcotic drug.
Who writes the recipe?
- oncologist
- district therapist,
- doctor of any specialty who was trained to work with narcotic and psychotropic substances.
How long does the recipe work?
15 days. Enough for any "holidays". But if he is needed urgently, then he can be discharged both on a holiday and on a holiday.
Do I need to take ampoules?
Not. By law, no one has the right to require the patient or his family to donate used ampoules, patches and packaging from narcotic analgesics.
Can one of the relatives get a prescription and a drug on behalf of the patient?
- To write a prescription, the doctor must conduct an inspection. But if the patient cannot reach the hospital, he has the right to call the doctor at home.
- For the seal, you still have to send someone from your relatives to the clinic - the seal of the medical institution on the recipe is obligatory.
- Both the patient and his authorized representative (with a passport and a copy of the patient's passport) can receive the drug at a specially designated pharmacy
What should I do if I am having difficulty getting an anesthetic?
- Call the hotline of the Ministry of Health: 8-800-200-03-89,
- Roszdravnadzor: 8-800-500-18-35,
- In the insurance company, which issued your policy OMS.
In conclusion, I want to somehow summarize everything said on this difficult topic:
- The pain can not be tolerated! You should not be afraid of the words “narcotic analgesics”, with a reasonable approach and following the recommendations of a competent doctor, the patient does not risk forming an addiction. According to the information letters of the Ministry of Health of the Russian Federation, all patients should be anesthetized.
- Modern painkillers in combination with adjuvant drugs give the doctor a lot of options to successfully arrest the pain syndrome. The serious baggage of experience of Medicine 24/7 confirms: even in the final stages of the oncological process, even in incurable patients, there is almost always the opportunity to keep a person clear and have a normal quality of life without suffering.
- Over the past 4 years, the procedure for obtaining drugs for patients has been somewhat simplified, although for the budgetary medical institutions themselves everything is still extremely bureaucratic. They abolished the Federal Drug Control Service, which also made life easier for doctors. Yes, there is plenty of work ahead. For example, to form, finally, a unified register of patients who need narcotic analgesics, which has been talked about since 2015. But there are shifts in the direction of facilitating the procedure for obtaining prescription painkillers in Russia.
Let nothing else hurt you for a very, very long time!
Source: https://habr.com/ru/post/437782/