Back pain - understanding from the perspective of modern medicine
People’s poor understanding of the causes of back pain has pushed me to adapt my recently published review of lower back pain for a wider reader.
Attention! This post does not encourage self-medication and self-diagnosis, is not of an advertising nature and serves exclusively educational purposes.

Despite the emphasis on pain in the lumbar region as a whole, everything written is applicable in the context of pain and in other parts of the spine.
Lower back pain (pain in the lumbar spine, UA) is one of the most common pathologies in the adult population and, according to some sources, occurs in more than 80% of the population. Acute pain syndrome lasts up to 6 weeks, subacute course - up to 12, chronic UA, with a duration of more than 3 months. According to Russian studies, acute pain in the lower back was experienced at least once during the life of up to 90% of the population.
Complaints of UAs can be caused by overloading of muscles and ligaments, bone tissue and facet (intervertebral) joints, hip joint, pelvic organs and abdominal organs. Psychological factors often play a role in the formation of chronic BAH: stress, depression and anxiety. There are certain genetic pathologies (neuromuscular diseases), the main and only manifestation of which may be pain syndrome in the back muscles.
About 80–85% of cases of UA are non-specific pain, the causes of which are problems of the muscles, facet (intervertebral) joints, ligaments of the sacroiliac joint. In 10–15% of cases, radicular pain (“gives up” along the nerve), accompanies the symptoms of compression of the nerve root or stenosis of the spinal canal - in such cases most often there will be muscle weakness and impaired sensitivity of part of the skin (respectively, “nourishment” by the nerve). Up to 1–5% is due to specific pain associated with the pathology of bone tissue (fractures, tumors, etc.), articular and periarticular (rheumatological diseases) and distant structures (reflected visceral pain, aortic aneurysm, etc.), with neuromuscular diseases.
With specific pain, which requires in-depth examination and consultation of relevant specialists, a system of “red flags” has been developed - symptoms that require special alertness:
Patients with radicular pain (i.e. along the nerve root) require consultation with a neurologist and a neurosurgeon with mandatory additional instrumental examinations: an MRI (most often) or a CT scan (less often because it poorly visualizes possible hernias) as prescribed by a specialist. In difficult situations, it makes sense to conduct a myography (usually needle-like) - but this is solely on the doctor’s prescription.
Facet pain syndrome accounts for up to 30% of all cases of UA. It is caused by changes characteristic of arthrosis of intervertebral joints. The facet syndrome may be present in other diseases - spondyloarthritis (psoriatic, Bechterew's disease), rheumatoid arthritis, gift and other metabolic disorders, the consequences of traumatic injuries. According to experts, the frequency of damage to the facet joints with back pain reaches 40–85% and increases with age.
Normally, the articular surfaces and capsules of these joints allow a certain amount of movement with a small amplitude. However, changes in the height and density of the intervertebral disc or changes in posture with the formation of excessive deflection (hyperlordosis) in the lumbar region lead to the fact that the usual movements in the spine exceed the physiological capabilities of the facet joints, increasing the load on them and increasing the tension of the joint capsules. These articular structures have a good “nerve supply” (innervation), therefore, when they are damaged, persistent irritation of pain receptors is formed. Clinically, facet syndrome usually presents with pain in the lumbar spine over the affected joint; pain "gives" in the hip or groin area. Unlike radicular syndrome, facet pain does not spread below the popliteal fossa. Characterized by the dynamics of pain during the day. Often appears in the morning and decreases after physical activity (patients note that “it is necessary to disperse”). But then it usually increases again after a prolonged static load, extension in the lumbar spine, tilt and rotation to the affected side, changing body position and is facilitated by slight bending, in a sitting position, supported by a railing or stand, in a lying position on a flat surface slightly bent legs in hip and knee joints.
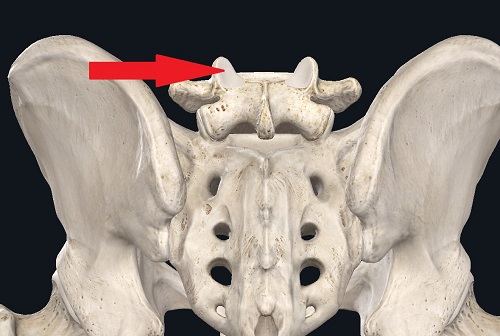
Those facets - intervertebral - joints.
The pain associated with muscle spasm is second in frequency and usually also depends on dynamic and static overload due to changes in posture. Sometimes there are secondary muscle spasms - due to local instability of the vertebral motor segment (two vertebrae and a disk between them), which is usually additionally accompanied by facet pain syndrome. Muscle pain is fairly easy to diagnose after determining the specific muscle suffering - the pain increases with stretching or stress on this individual muscle in a certain movement.
Pain in the sacroiliac joint can also be acute or chronic. The cause of the pain syndrome is not completely clear. It is believed that pain can occur when the capsular-ligamentous apparatus of the joint is stretched, hyper or hypomobile and changes in the biomechanical loads and movements in the joint, which leads to inflammation.

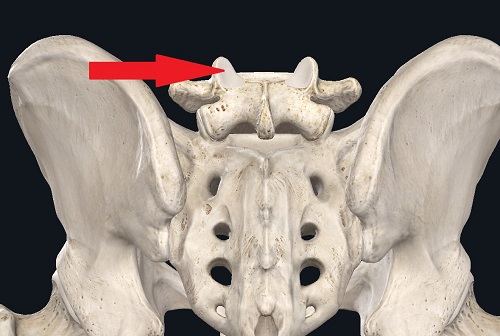
Ligaments of the sacroiliac joint.
There are a huge number of reasons for back pain. Most often, the pain is nonspecific, local, associated with dynamic overload and / or inflammation in the intervertebral (faceted) joints, sprains of the sacroiliac joint, or muscle spasm, and does not require a specific MRI / CT scan. According to Russian recommendations (which, by the way, are written correctly enough - precisely for lower back pain for general practitioners), x-rays are recommended to be taken only if pain persists for more than a month or for constant relapses. We must not forget about the possibility of back pain due to hip joint arthrosis - in this case, the entire biomechanics of the lower limb and pelvis may change, overloading the lower back for the second time. In this case, it is useless to treat the lower back.
The choice of treatment tactics primarily depends on an understanding of the pathogenesis of the pain syndrome. It is always based on the inflammatory component. In large-scale placebo-controlled studies confirmed the effectiveness of the appointment of nonsteroidal anti-inflammatory drugs, as the "gold standard" for the treatment of acute pain syndromes. It is advisable to prescribe the drug on average for 3-4 weeks, depending on the intensity and duration of pain, however, the course should be at least 2 weeks. Since in addition to achieving a more rapid analgesic effect, it is necessary to stop the inflammatory process, which requires a longer period of treatment. In such cases, a slightly higher dose is usually given for the first 3-5-7 days (for the sake of pain relief + anti-inflammatory effect), then the dose is reduced to maintain the anti-inflammatory effect.
Conservative treatment of non-specific BVS is diverse. Drug therapy for diabetes patients includes the appointment of tricyclic antidepressants (level of evidence B), muscle relaxants (level of evidence B), NSAIDs (level of evidence B), paracetamol (level of evidence B). From non-drug methods, therapeutic physical training (level of evidence B), manual therapy (level of evidence B), psychotherapy at the stage of rehabilitation after eliminating the organic cause (level of evidence B) are effective.
It is not recommended to limit daily physical activity and use corsets, as this may lead to an increase in the terms of pain syndrome.
Since I have a second manual therapist certificate, I can write about manual therapy in the treatment of back pain. Below will be partly my thoughts, partly - information from the recommendations.
Manual therapy is a set of manipulations that may or may not be effective for back pain. That is, it is a skill that well complements the main specialty such as traumatology and orthopedics, neurology or sports medicine and exercise therapy. Two points follow from this.
Firstly, from my personal point of view, manual therapy should not be a separate specialty - especially now that it can be obtained by a single certificate after the institute. We do not have separate specialists for intra-articular injections, for droppers, for the purpose of the orthoses, respectively, it is somewhat wrong that manual therapy received a separate certificate.
Secondly, judging by the recommendations of both ours and the bourgeoisie (including information from the cochrane), manual therapy is not inferior in efficiency, but does not exceed other methods of treatment, including drug therapy or physical therapy. From my experience and my practice, MT has no long-term effect. Long-term - only a modification of lifestyle and physical therapy, or even physical activity. In fact, MT will help someone, someone won't. And she has no preventive action, as this is just one of the methods for treating back pain. The only BUT here you can specify only one option in my opinion - if you regularly do physical therapy with a doctor , and he himself, having a manual therapist certificate, periodically combines it with physiotherapy exercises. Here, logically, there should be a good enough effect.
I repeat, even though it was said above - psychological / mental status may be associated with the appearance and presence of back pain.
Neuromuscular diseases can have only back pain in the manifestations - most often such patients suffer from back pain for many years with a short-term effect from various activities.
If the pain is local only in the back - you should not run to do an MRI, most likely this is not required, and the x-ray will be enough for the doctor.
References can be viewed in a small review, which is published in a scientific journal under my authorship (the journal Neuromuscular Diseases, included in the list of HAC and in the Scopus database).
Link to the original article in the journal
Attention! This post does not encourage self-medication and self-diagnosis, is not of an advertising nature and serves exclusively educational purposes.

Despite the emphasis on pain in the lumbar region as a whole, everything written is applicable in the context of pain and in other parts of the spine.
Lower back pain (pain in the lumbar spine, UA) is one of the most common pathologies in the adult population and, according to some sources, occurs in more than 80% of the population. Acute pain syndrome lasts up to 6 weeks, subacute course - up to 12, chronic UA, with a duration of more than 3 months. According to Russian studies, acute pain in the lower back was experienced at least once during the life of up to 90% of the population.
Complaints of UAs can be caused by overloading of muscles and ligaments, bone tissue and facet (intervertebral) joints, hip joint, pelvic organs and abdominal organs. Psychological factors often play a role in the formation of chronic BAH: stress, depression and anxiety. There are certain genetic pathologies (neuromuscular diseases), the main and only manifestation of which may be pain syndrome in the back muscles.
About 80–85% of cases of UA are non-specific pain, the causes of which are problems of the muscles, facet (intervertebral) joints, ligaments of the sacroiliac joint. In 10–15% of cases, radicular pain (“gives up” along the nerve), accompanies the symptoms of compression of the nerve root or stenosis of the spinal canal - in such cases most often there will be muscle weakness and impaired sensitivity of part of the skin (respectively, “nourishment” by the nerve). Up to 1–5% is due to specific pain associated with the pathology of bone tissue (fractures, tumors, etc.), articular and periarticular (rheumatological diseases) and distant structures (reflected visceral pain, aortic aneurysm, etc.), with neuromuscular diseases.
With specific pain, which requires in-depth examination and consultation of relevant specialists, a system of “red flags” has been developed - symptoms that require special alertness:
- age of patient over 50–55 years or under 18–20 years;
- pain is not associated with movement, is combined with pain in another location and / or is common (more than one root suffers);
- a serious spinal injury or connection of the onset of the disease with a previous injury;
- persistent fever;
- the presence of cancer in history;
- unexplained weight loss;
- persistent at night or constantly progressive back pain;
- increasing neurological symptoms - urinary incontinence or difficulty urinating, “saddle-like” loss of sensation in the anus and perineum, bilateral weakness and / or numbness of the lower extremities, impotence);
- pulsating formation in the abdominal cavity;
- backache, aggravated at rest;
- immunosuppression, immunodeficiency virus, drug addiction;
- long-term use of glucocorticoids (hormones);
- the presence of systemic diseases;
- increase in pain over time;
- lack of relief and reduction of back pain after lying down;
- intense and daily pain predominantly in the thoracic spine;
- spinal deformity, formed in a short time;
- the general condition of the patient with a long malaise suffers.
Patients with radicular pain (i.e. along the nerve root) require consultation with a neurologist and a neurosurgeon with mandatory additional instrumental examinations: an MRI (most often) or a CT scan (less often because it poorly visualizes possible hernias) as prescribed by a specialist. In difficult situations, it makes sense to conduct a myography (usually needle-like) - but this is solely on the doctor’s prescription.
Facet pain syndrome accounts for up to 30% of all cases of UA. It is caused by changes characteristic of arthrosis of intervertebral joints. The facet syndrome may be present in other diseases - spondyloarthritis (psoriatic, Bechterew's disease), rheumatoid arthritis, gift and other metabolic disorders, the consequences of traumatic injuries. According to experts, the frequency of damage to the facet joints with back pain reaches 40–85% and increases with age.
Normally, the articular surfaces and capsules of these joints allow a certain amount of movement with a small amplitude. However, changes in the height and density of the intervertebral disc or changes in posture with the formation of excessive deflection (hyperlordosis) in the lumbar region lead to the fact that the usual movements in the spine exceed the physiological capabilities of the facet joints, increasing the load on them and increasing the tension of the joint capsules. These articular structures have a good “nerve supply” (innervation), therefore, when they are damaged, persistent irritation of pain receptors is formed. Clinically, facet syndrome usually presents with pain in the lumbar spine over the affected joint; pain "gives" in the hip or groin area. Unlike radicular syndrome, facet pain does not spread below the popliteal fossa. Characterized by the dynamics of pain during the day. Often appears in the morning and decreases after physical activity (patients note that “it is necessary to disperse”). But then it usually increases again after a prolonged static load, extension in the lumbar spine, tilt and rotation to the affected side, changing body position and is facilitated by slight bending, in a sitting position, supported by a railing or stand, in a lying position on a flat surface slightly bent legs in hip and knee joints.
Those facets - intervertebral - joints.
The pain associated with muscle spasm is second in frequency and usually also depends on dynamic and static overload due to changes in posture. Sometimes there are secondary muscle spasms - due to local instability of the vertebral motor segment (two vertebrae and a disk between them), which is usually additionally accompanied by facet pain syndrome. Muscle pain is fairly easy to diagnose after determining the specific muscle suffering - the pain increases with stretching or stress on this individual muscle in a certain movement.
Pain in the sacroiliac joint can also be acute or chronic. The cause of the pain syndrome is not completely clear. It is believed that pain can occur when the capsular-ligamentous apparatus of the joint is stretched, hyper or hypomobile and changes in the biomechanical loads and movements in the joint, which leads to inflammation.

Ligaments of the sacroiliac joint.
Short summary + several additions
There are a huge number of reasons for back pain. Most often, the pain is nonspecific, local, associated with dynamic overload and / or inflammation in the intervertebral (faceted) joints, sprains of the sacroiliac joint, or muscle spasm, and does not require a specific MRI / CT scan. According to Russian recommendations (which, by the way, are written correctly enough - precisely for lower back pain for general practitioners), x-rays are recommended to be taken only if pain persists for more than a month or for constant relapses. We must not forget about the possibility of back pain due to hip joint arthrosis - in this case, the entire biomechanics of the lower limb and pelvis may change, overloading the lower back for the second time. In this case, it is useless to treat the lower back.
Treatment
The choice of treatment tactics primarily depends on an understanding of the pathogenesis of the pain syndrome. It is always based on the inflammatory component. In large-scale placebo-controlled studies confirmed the effectiveness of the appointment of nonsteroidal anti-inflammatory drugs, as the "gold standard" for the treatment of acute pain syndromes. It is advisable to prescribe the drug on average for 3-4 weeks, depending on the intensity and duration of pain, however, the course should be at least 2 weeks. Since in addition to achieving a more rapid analgesic effect, it is necessary to stop the inflammatory process, which requires a longer period of treatment. In such cases, a slightly higher dose is usually given for the first 3-5-7 days (for the sake of pain relief + anti-inflammatory effect), then the dose is reduced to maintain the anti-inflammatory effect.
Conservative treatment of non-specific BVS is diverse. Drug therapy for diabetes patients includes the appointment of tricyclic antidepressants (level of evidence B), muscle relaxants (level of evidence B), NSAIDs (level of evidence B), paracetamol (level of evidence B). From non-drug methods, therapeutic physical training (level of evidence B), manual therapy (level of evidence B), psychotherapy at the stage of rehabilitation after eliminating the organic cause (level of evidence B) are effective.
It is not recommended to limit daily physical activity and use corsets, as this may lead to an increase in the terms of pain syndrome.
Total treatment
- No need to be treated independently. General practitioners, some orthopedic traumatologists and neurologists are the specialists who (in theory) should be able to examine a patient with back pain and prescribe treatment.
- Standard therapy is anti-inflammatory and painkillers + muscle relaxants in cases of marked muscle spasm. In cases of instability, muscle relaxants can worsen the situation, so their use is not always advisable.
- In cases of marked pain syndrome, hormonal drugs can be used (even without nerve compression). There will be nothing bad from a few droppers, so there is no need to be afraid of them. But long-term administration should be avoided + in no case apply them yourself.
- Vitamins of group B, "vascular" drugs, etc. they are not even included in the domestic standards of treatment and do not have any evidence of back pain.
- The use of corsets is almost always impractical, as is the restriction of daily activity. It is everyday household - go to the gym with back pain or unload the car with bags of cement is not worth it.
- The best long-term prevention strategy is lifestyle modification — weight loss, correction of concomitant diseases such as obesity or flatfoot, and rational exercise. At the stage from “not so painfully, I can move” to “it does not hurt, I want prophylaxis” one of the most correct choices is therapeutic exercise under the supervision of an adequate rehabilitologist / physician
- The applicability of physiotherapy leave on the conscience of doctors. I can only note that in the same US I have personally met two proven methods in the same USA - phonophoresis with hydrocortisone and shock wave therapy.
Since I have a second manual therapist certificate, I can write about manual therapy in the treatment of back pain. Below will be partly my thoughts, partly - information from the recommendations.
Manual therapy is a set of manipulations that may or may not be effective for back pain. That is, it is a skill that well complements the main specialty such as traumatology and orthopedics, neurology or sports medicine and exercise therapy. Two points follow from this.
Firstly, from my personal point of view, manual therapy should not be a separate specialty - especially now that it can be obtained by a single certificate after the institute. We do not have separate specialists for intra-articular injections, for droppers, for the purpose of the orthoses, respectively, it is somewhat wrong that manual therapy received a separate certificate.
Secondly, judging by the recommendations of both ours and the bourgeoisie (including information from the cochrane), manual therapy is not inferior in efficiency, but does not exceed other methods of treatment, including drug therapy or physical therapy. From my experience and my practice, MT has no long-term effect. Long-term - only a modification of lifestyle and physical therapy, or even physical activity. In fact, MT will help someone, someone won't. And she has no preventive action, as this is just one of the methods for treating back pain. The only BUT here you can specify only one option in my opinion - if you regularly do physical therapy with a doctor , and he himself, having a manual therapist certificate, periodically combines it with physiotherapy exercises. Here, logically, there should be a good enough effect.
I repeat, even though it was said above - psychological / mental status may be associated with the appearance and presence of back pain.
Neuromuscular diseases can have only back pain in the manifestations - most often such patients suffer from back pain for many years with a short-term effect from various activities.
If the pain is local only in the back - you should not run to do an MRI, most likely this is not required, and the x-ray will be enough for the doctor.
References can be viewed in a small review, which is published in a scientific journal under my authorship (the journal Neuromuscular Diseases, included in the list of HAC and in the Scopus database).
Link to the original article in the journal
Source: https://habr.com/ru/post/439794/